Day 1 :
- Innovation and Research in Otology
Session Introduction
Dr. Lee Akst
Johns Hopkins University. USA
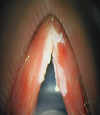
Title: Vocal Cord Leukoplakia: Management in the OR and Office

Biography:
Dr. Lee Akst is head of the Johns Hopkins Voice Center and is Director of the Division of Laryngology at the Johns Hopkins University Department of Otolaryngology-Head and Neck Surgery. The focus of his clinical practice is on management of voice disorders, with focus on office-based treatments and operative management of epithelial diseases such as vocal cord leukoplakia, papilloma, and early glottis cancer. He has lectured extensively on phonosurgical techniques, treatment of laryngeal leukoplakia, laryngopharyngeal reflux, and globus pharyngeus. He has been working with engineers at Johns Hopkins on novel robotic platforms to bringing robotic surgery into the endolarynx to aid microlaryngeal operative precision. Dr. Akst received his undergraduate and medical degrees from Yale University, did his Otolaryngology residency at the Cleveland Clinic, and completed his laryngology fellowship at Massachusetts General Hospital.
Abstract:
This presentation will comprehensively review evaluation and management of laryngeal leukoplakia. Though “white vocal fold lesions” are common, management remains challenging – doing ‘too little’ may allow precancerous lesions to progress, while doing ‘too much’ may create unnecessary dysphonia through scar. I will present a framework for management of leukoplakia which balances oncologic with functional outcomes, with the goal of achieving disease control without creating scar. State-of-the-art advances in care of leukoplakia will be emphasized, and surgical techniques discussed will include role of infusion, use of the KTP laser, and microflap resection of diseased epithelium. Advanced use of the KTP laser for office treatment of laryngeal dysplasia, an important part of my own practice and something which is only available in a limited number of centers worldwide, will be discussed as well, to include appropriate anesthesia techniques for office-based procedures. Epidemiology of leukoplakia, rates of progression to malignancy, and role of office-based biopsy will be reviewed.
Though focus will be on KTP laser strategies as these represent cutting edge approached to management of this disease, I will also discuss cold instrument and CO2 laser techniques so that the audience, regardless of the tools available to them in their own practices, will be able to transition techniques learned in this presentation to care of their own patients. Approaches to anterior commissure involvement, bilateral disease, and multiply recurrent dysplasia will be discussed through case presentations which should increase audience interest.
Learning Objectives: “At the completion of this presentation, participants should be able to:”
1. Understand the need to balance oncologic efficacy with functional outcomes in leukoplakia care.
2. Discuss treatment alternatives for laryngeal leukoplakia, emphasizing surgical techniques of KTP, CO2, and cold-instrument phonosurgery in the operating room and pulsed KTP laser treatment in an office setting.
- Head and Neck Surgery and Oncology
Session Introduction
Produl Hazarika
NMC Specialty Hospital. UAE
Title: SURGICAL APPROACHES FOR JUVENILE NASOPHARYNGEAL ANGIOFIBROMA –SPECTRUM ANALYSIS.

Biography:
Prof Produl Hazarika MBBS, DLO, MS, FACS, FRCS (Edin), FIAO, FUWAI, Fellow of UICC is presently working as an otolaryngologist in NMC Specialty Hospital in Abu Dhabi, U.A.E. He is a former professor and head and director of post graduate studies of the department of Otorhinolaryngology and Head & Neck Surgery in Kasturba Medical College, Manipal, India. He has 28 years of clinical teaching experience both at the undergraduate and postgraduate levels, with over 100 publications in various national and international journals. He was selected as international guest scholar by the American College of Surgeon in 1986 and has travelled widely to the U.S, Australia, U.K and Malaysia, Switzerland, Mauritius on various fellowship programs.
Abstract:
Juvenile nasopharyngeal angiofiboma (JNA) is a very rare benign vascular tumor, occurs, only in adolescent male. 0.5% of all head &neck tumors are JNA. Presenting symptoms of this tumor are profuse, painless, unprovoked, recurrent nasal bleeding. Nasal obstruction in early cases but myriad of symptoms ‘of facial swelling , proptosis and other neurological symptoms may be seen in late cases. JNA though originally arises from nasopharynx also is very much known for its extension to the different parts of the nose, skull base and intracranial spaces, causing both diagnostic and therapeutic problem for the practicing otolaryngologist. Common clinical presentation of these tumors is nasal obstruction in 80 to 90 percent followed by recurrent, painless, profuse and unprovoked epistaxis in 45 to 60 percent of the cases. Radiological investigations included are contrast Ct scan, MRI scan, angiography to find the feeding vessel. Surgical removal of the tumor is the only definitive line of treatment. However, various surgical approaches may be needed depending on its extension and vascular supply. This paper deals with 33 cases of JNA with or without extra nasopharyngeal extension where ten different surgical approaches have been adopted for tumor excision. Logic of application and advantages of surgical procedure in each case of angiofibroma will be highlighted and will be demonstrated in video clip. Newer approaches like endoscopic and Le forte osteotomy will be discussed more in details. Recurrence after surgery, avoidance and treatment will also be discussed.
Produl Hazarika
NMC Specialty Hospital. UAE
Title: SURGICAL APPROACHES FOR JUVENILE NASOPHARYNGEAL ANGIOFIBROMA –SPECTRUM ANALYSIS.

Biography:
Prof Produl Hazarika MBBS, DLO, MS, FACS, FRCS (Edin), FIAO, FUWAI, Fellow of UICC is presently working as an otolaryngologist in NMC Specialty Hospital in Abu Dhabi, U.A.E. He is a former professor and head and director of post graduate studies of the department of Otorhinolaryngology and Head & Neck Surgery in Kasturba Medical College, Manipal, India. He has 28 years of clinical teaching experience both at the undergraduate and postgraduate levels, with over 100 publications in various national and international journals. He was selected as international guest scholar by the American College of Surgeon in 1986 and has travelled widely to the U.S, Australia, U.K and Malaysia, Switzerland, Mauritius on various fellowship programs.
Abstract:
Juvenile nasopharyngeal angiofiboma (JNA) is a very rare benign vascular tumor, occurs, only in adolescent male. 0.5% of all head &neck tumors are JNA. Presenting symptoms of this tumor are profuse, painless, unprovoked, recurrent nasal bleeding. Nasal obstruction in early cases but myriad of symptoms ‘of facial swelling , proptosis and other neurological symptoms may be seen in late cases. JNA though originally arises from nasopharynx also is very much known for its extension to the different parts of the nose, skull base and intracranial spaces, causing both diagnostic and therapeutic problem for the practicing otolaryngologist. Common clinical presentation of these tumors is nasal obstruction in 80 to 90 percent followed by recurrent, painless, profuse and unprovoked epistaxis in 45 to 60 percent of the cases. Radiological investigations included are contrast Ct scan, MRI scan, angiography to find the feeding vessel. Surgical removal of the tumor is the only definitive line of treatment. However, various surgical approaches may be needed depending on its extension and vascular supply. This paper deals with 33 cases of JNA with or without extra nasopharyngeal extension where ten different surgical approaches have been adopted for tumor excision. Logic of application and advantages of surgical procedure in each case of angiofibroma will be highlighted and will be demonstrated in video clip. Newer approaches like endoscopic and Le forte osteotomy will be discussed more in details. Recurrence after surgery, avoidance and treatment will also be discussed.
Alessandro Bucci
ENT Department – Senigallia. Italy
Title: Endoscopic evaluation during sleep of airway obstruction in OSAS: an update on recent literature and our personal in experience

Biography:
Alessandro Bucci is a Reserve Medical Officer of Italian Navy. He has Fellowship experienced in Otolaryngology at University Hospital, Cadiz, Spain. He was a Consultant in Otolaryngology. He has Fellowship in Facial Plastic Surgery (AMC) and OSAS at Sint Lucas Andreas Hospital, Amsterdam, Netherlands and in Facial Plastic Surgery at C. Garcia University Hospital, Cuba. He is a dedicated ENT Specialist Surgeon with 14 years of experience providing the highest standard of treatment. His research focused on rhinology/rhinoallergology, OSAS and dysphagia.
Abstract:
Obstructive sleep apnea (OSA) is a sleep disorder that involves cessation or significant decrease in airflow in the presence of breathing effort. Airway obstruction in OSA can occur at many levels. Surgical procedures are inherently directed at specific regions of the upper airway. Traditionally, upper airway examination is performed while the patient is awake. Nasofibrolaryngoscopy under induced sleep is a promising alternative for identifying sites of upper airway obstruction in patients with OSA. The purpose of this study was to systematically review the evidence regarding the usefulness of Drug Induced Sleep Endoscopy (DISE) compared with that of traditional awake examination for surgical decision- making in patients with OSAS. This review emphasized the direct impact of DISE compared with that of awake examination on surgical decision-making in OSA patients.
Materials and methods used. DISE has been used as a method of evaluation of the upper airway during pharmacologically induced sleep. During DISE artificial sleep is induced by propofol, and the pharyngeal collapse patterns are visualized using a flexible fiberoptic nasopharyngoscope. A systematic review was performed of studies using DISE to identify obstruction sites and patterns of obstruction in patients with OSA. The level (palate, oropharynx, tongue base, hypopharynx/epiglottis), the direction (antero-posterior, concentric, lateral), and the degree of collapse were scored according to the NOHL classification. Only studies with a primary objective of evaluating the usefulness of DISE for surgical decision-making and the importance of identifying multilevel obstruction were selected. Then a retrospective chart review of OSAS patients who underwent DISE at our Centre for Diagnosis and Treatment of Respiratory Sleep Disorders, as part of their surgical evaluation, were reviewed. We compared the results of clinical and diagnostic evaluation with those of sleep endoscopy. According to others authors we found that palatal obstruction was the most frequently observed site of obstruction, followed by tongue base obstruction, laryngeal obstruction and hypopharyngeal obstruction.
Conclusion. Although consensus has been reached on several aspects of the DISE procedure some topics remain open to future research. DISE is an additional method to reveal obstruction sites that have not been detected in awake patients. DISE is mandatory in the diagnostic work-up of OSA and is a valid addition when surgery is considered. DISE is a dynamic, safe, and easy-to-perform technique that visualizes the anatomical sites of snoring or apnoeas. Anyway, larger detailed analyses are needed to determine the importance of each site and degree of obstruction seen on DISE.
- Laryngology

Chair
Lee Akst
Johns Hopkins University
Session Introduction
Lee Akst
Johns Hopkins University, USA.
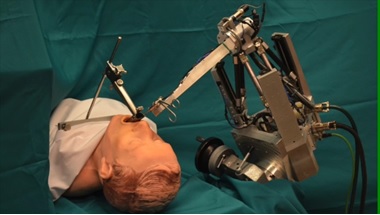
Title: Evolutions in Robotic Microlaryngeal Surgery

Biography:
Dr. Lee Akst is head of the Johns Hopkins Voice Center and is Director of the Division of Laryngology at the Johns Hopkins University Department of Otolaryngology-Head and Neck Surgery. The focus of his clinical practice is on management of voice disorders, with focus on office-based treatments and operative management of epithelial diseases such as vocal cord leukoplakia, papilloma, and early glottis cancer. He has lectured extensively on phonosurgical techniques, treatment of laryngeal leukoplakia, laryngopharyngeal reflux, and globus pharyngeus. He has been working with engineers at Johns Hopkins on novel robotic platforms to bringing robotic surgery into the endolarynx to aid microlaryngeal operative precision. Dr. Akst received his undergraduate and medical degrees from Yale University, did his Otolaryngology residency at the Cleveland Clinic, and completed his laryngology fellowship at Massachusetts General Hospital.
Abstract:
This presentation will review limitations of current robotic approaches to microlaryngoscopy, and will introduce the audience to a new robotic technology with the potential to change how microlaryngeal surgeries are performed. The evolution of laryngeal surgical techniques have been driven by the promise of increased operative precision. Coincident with advances in microlaryngeal surgery have been similar, though more rapid, advances in robot-assisted surgery within Otolaryngology. From well-established use of the da Vinci surgical robot for ablative procedures of the pharynx to newer applications for robot-assisted procedures such as thyroid surgery and skull base surgery, robotic-assisted surgery is growing.
Despite these advances, robot-assisted surgery is not yet routinely incorporated into microlaryngeal surgery. Current limitations for existing commercial systems include size of available instrumentation, difficulty manipulating robotic effector arms within narrow working space afforded by standard retractors, and reduced haptic feedback that comes from working remotely rather than handling tissues directly. Even as smaller instruments and new retractors are being developed, existing robots have been largely limited to laryngeal procedures such as vocal cord stripping, cordectomy, and partial epiglottectomy – procedures in which preservation of normal vocal fold anatomy and function are not prioritized.
To address these issues and create a role for robotic assistance in microlaryngoscopy, a novel robotic ENT microsurgery system (REMS) has been developed. This system emphasizes cooperative control, rather than remote control, of a microsurgical instrument; traditional microlaryngoscopy instruments are utilized with both the robot arm and surgeon controlling the same instrument. The ability of this REMS system to improve precise performance of simulated microlaryngoscopy tasks has been demonstrated in a variety of research studies. These preliminary studies, their methods, and their results will be reviewed; surgical videos will demonstrate the robot ‘in action’. The REMS platform may represent the next step in the evolution of robotic microlaryngeal surgery.
Alessandro Bucci
ENT Department – Senigallia, Italy
Title: Endoscopic evaluation during sleep of airway obstruction in OSAS: an update on recent literature and our personal in experience

Biography:
Alessandro Bucci is a Reserve Medical Officer of Italian Navy. He has Fellowship experienced in Otolaryngology at University Hospital, Cadiz, Spain. He was a Consultant in Otolaryngology. He has Fellowship in Facial Plastic Surgery (AMC) and OSAS at Sint Lucas Andreas Hospital, Amsterdam, Netherlands and in Facial Plastic Surgery at C. Garcia University Hospital, Cuba. He is a dedicated ENT Specialist Surgeon with 14 years of experience providing the highest standard of treatment. His research focused on rhinology/rhinoallergology, OSAS and dysphagia.
Abstract:
Obstructive sleep apnea (OSA) is a sleep disorder that involves cessation or significant decrease in airflow in the presence of breathing effort. Airway obstruction in OSA can occur at many levels. Surgical procedures are inherently directed at specific regions of the upper airway. Traditionally, upper airway examination is performed while the patient is awake. Nasofibrolaryngoscopy under induced sleep is a promising alternative for identifying sites of upper airway obstruction in patients with OSA. The purpose of this study was to systematically review the evidence regarding the usefulness of Drug Induced Sleep Endoscopy (DISE) compared with that of traditional awake examination for surgical decision- making in patients with OSAS. This review emphasized the direct impact of DISE compared with that of awake examination on surgical decision-making in OSA patients.
Materials and methods used. DISE has been used as a method of evaluation of the upper airway during pharmacologically induced sleep. During DISE artificial sleep is induced by propofol, and the pharyngeal collapse patterns are visualized using a flexible fiberoptic nasopharyngoscope. A systematic review was performed of studies using DISE to identify obstruction sites and patterns of obstruction in patients with OSA. The level (palate, oropharynx, tongue base, hypopharynx/epiglottis), the direction (antero-posterior, concentric, lateral), and the degree of collapse were scored according to the NOHL classification. Only studies with a primary objective of evaluating the usefulness of DISE for surgical decision-making and the importance of identifying multilevel obstruction were selected. Then a retrospective chart review of OSAS patients who underwent DISE at our Centre for Diagnosis and Treatment of Respiratory Sleep Disorders, as part of their surgical evaluation, were reviewed. We compared the results of clinical and diagnostic evaluation with those of sleep endoscopy. According to others authors we found that palatal obstruction was the most frequently observed site of obstruction, followed by tongue base obstruction, laryngeal obstruction and hypopharyngeal obstruction.
Conclusion. Although consensus has been reached on several aspects of the DISE procedure some topics remain open to future research. DISE is an additional method to reveal obstruction sites that have not been detected in awake patients. DISE is mandatory in the diagnostic work-up of OSA and is a valid addition when surgery is considered. DISE is a dynamic, safe, and easy-to-perform technique that visualizes the anatomical sites of snoring or apnoeas. Anyway, larger detailed analyses are needed to determine the importance of each site and degree of obstruction seen on DISE.
Zeyad mandour
Alexandria University, EGYPT.
Title: To evaluate endoscopic closure of nasal septal perforation using pedicled inferior turbinate flap

Biography:
Oto-rhino-laryngology and Head & Neck Surgery M.D -Consultant of Endoscopic Sinus Surgery & Microscopic Ear Surgery -ORL Professor, Alexandria University -- Fellowship Marseilles- France.
Abstract:
Septal perforations are usually difficult to treat. Surgery is indicated if the perforation is symptomatic. Our aim is to evaluate endoscopic closure of nasal septal perforation using pedicled inferior turbinate flap.
Patients and Methods: Endoscopic closure of nasal septum perforations were performed in 31 patients using unilateral pedicled inferior turbinate flap.
Results: Twenty-three patients (74%) had complete closure of their perforations. Six other patients (19.5%) had incomplete closure with a small residual perforation< 1cm in diameter posteriorly. Two patients (6.5%), who had previous submucosal diathermy of the inferior turbinate, had flap necrosis with complete failure of the repair. There was a significant inverse relationship between the diameter of the perforation and the success of the repair.
Conclusions: Endoscopic repair of nasal septal perforations, up to 2 cm in diameter, using a modified pedicled inferior turbinate flap, is a feasible technique that offers acceptable success rates due to the remarkable vascularity and thickness of the flap. The use of endoscopes allowed more precise a traumatic elevation of the flap posteriorly. The present technique differs from other previously described flap procedures in that it extends the posterior dissection to include a part of the mucosa of the inferior meatus in order to allow more free un-constrained rotation of the flap, and decrease the thickness of the pedicle so that we may not need to divide it in a second stage. This step would have been more difficult and less precise without the use of the endoscope. Previously operated turbinates are not suitable for this technique. Also the procedure may not be suitable if the perforation is very anterior or larger than 2 cm in diameter.
Keywords: Septum; Perforation; Endoscopic; Inferior turbinate flap
- Rhinology and Allergy
Session Introduction
Silvia Muriño
Parmenio Piñero Acute General Hospital, Argentina.
Title: Relationship between Immunodeficiencies, Allergy and Pathology of the Upper Airway

Biography:
ENT PhD and Allergy & Immunology practitioner, Parmenio Piñero Acute General Hospital (Buenos Aires City), F.A.S.O. Plenary member (Federación Argentina de Sociedades de Otorrinolaringología), A.O.C.B.A. Assistant Secretary, IAPO - Interamerican Association of Pediatric Otorhinolaryngology, American Academy of Otolaryngology-Head and Neck Surgery Intl Member, European Academy of Allergy & Clinical Immunology Intl Member
Abstract:
The respiratory system has defense mechanisms such as hair cells, Immune System, cough, sneezing, etc. Let's talk about the relationship between airway, allergy and immunodeficiency.
One of the most important substances to take into account is Histamine, both in its beneficial aspect and producing symptoms characteristic of these pathologies. IgE-mediated reactions, also present, involve mast cells and basophils.
The alteration of immunity and allergy is considered as a breakdown of the balance of the immune system. Let's not forget genetic and environmental factors (increased incidence in more urbanized communities)
We will also talk about the autonomic innervation that is so important to understand the symptomatology and its influence on the immune system and vice versa.
Arman Afrashi
Buca Seyfi Demirsoy State Hospital, Turkey.
Title: Pharyngolateral ferromagnetic prosthesis (PFP) for treatment of obstructive sleep apnea

Biography:
Abstract:
Obstructive sleep apnea is a disease consisting of episodes of partial or complete closure of the upper airway that occur during sleep and lead to breathing cessation defined as a period of apnea more than 10 s. Symptom include restlessness, snoring, recurrent awakening, morning head- ache and excessive day time sleepiness. Diagnosis of obstructive sleep apnea is based on sleep history and pol- ysomnography. Today the major treatment methods are continuous positive airway pressure, weight loss, positional therapy, oral appliances and different surgical procedures such as tracheostomy, nasal surgery, radiofre- quency of palatal region, soft palate implants, uvulophar- yngopalatoplasty, tongue base surgery, hyoid suspension, lateral pharyngoplasty, genioglossal advancement and maxillomandibular advancement.
In all of these surgical procedures except maxilloman- dibular advancement, the main problem is failure of pre- venting the collapse of lateral pharyngeal wall. In this new technique pharyngolateral ferromagnetic prosthesis will prevent the collapse of lateral pharyngeal wall during sleep.
Pharyngolateral ferromagnetic prosthesis: it contains two parts for each side of the pharyngeal part of the neck.
1. Internal part of prosthesis: it contains a fragmented thin part of a ferromagnetic material such as Iron (Fe), coated with biocompatible Silicone or another bio- compatible material.
2. External part of prosthesis: it contains a natural magnet with power between 6,000 and 10,000 Gauss. The external part of pharyngolateral ferromagnetic pros- thesis will use only during sleep in external part of the neck .
Surgical technique: patient will be in supine position and under general anesthesia during surgery. After inserting Davis-Boyle mouth gag, surgeon should make a 3-cm-long incision vertically in lateral wall of pharynx at the level of base of the tongue. Then surgeon should make dissection under mucosal and submucosal layers toward hypophar- ynx. After that he/she should insert the internal part of prosthesis and at the end close the incision . Then surgeon could perform the same procedure to the opposite side of the neck or perform unilaterally.
A few days after surgery patient should use the external part of the prosthesis in both sides of the neck during sleep. The magnetic power of external part of pros- thesis will pull the internal part of prosthesis and lateral hypopharyngeal wall together and this will prevent the collapse of lateral pharyngeal wall and obstructive attacks.
Lee Akst
Johns Hopkins University, USA.
Title: Vocal Cord Leukoplakia: Management in the OR and Office

Biography:
Dr. Lee Akst is head of the Johns Hopkins Voice Center and is Director of the Division of Laryngology at the Johns Hopkins University Department of Otolaryngology-Head and Neck Surgery. The focus of his clinical practice is on management of voice disorders, with focus on office-based treatments and operative management of epithelial diseases such as vocal cord leukoplakia, papilloma, and early glottis cancer. He has lectured extensively on phonosurgical techniques, treatment of laryngeal leukoplakia, laryngopharyngeal reflux, and globus pharyngeus. He has been working with engineers at Johns Hopkins on novel robotic platforms to bringing robotic surgery into the endolarynx to aid microlaryngeal operative precision. Dr. Akst received his undergraduate and medical degrees from Yale University, did his Otolaryngology residency at the Cleveland Clinic, and completed his laryngology fellowship at Massachusetts General Hospital.
Abstract:
This presentation will comprehensively review evaluation and management of laryngeal leukoplakia. Though “white vocal fold lesions” are common, management remains challenging – doing ‘too little’ may allow precancerous lesions to progress, while doing ‘too much’ may create unnecessary dysphonia through scar. I will present a framework for management of leukoplakia which balances oncologic with functional outcomes, with the goal of achieving disease control without creating scar. State-of-the-art advances in care of leukoplakia will be emphasized, and surgical techniques discussed will include role of infusion, use of the KTP laser, and microflap resection of diseased epithelium. Advanced use of the KTP laser for office treatment of laryngeal dysplasia, an important part of my own practice and something which is only available in a limited number of centers worldwide, will be discussed as well, to include appropriate anesthesia techniques for office-based procedures. Epidemiology of leukoplakia, rates of progression to malignancy, and role of office-based biopsy will be reviewed.
Though focus will be on KTP laser strategies as these represent cutting edge approached to management of this disease, I will also discuss cold instrument and CO2 laser techniques so that the audience, regardless of the tools available to them in their own practices, will be able to transition techniques learned in this presentation to care of their own patients. Approaches to anterior commissure involvement, bilateral disease, and multiply recurrent dysplasia will be discussed through case presentations which should increase audience interest.
Learning Objectives: “At the completion of this presentation, participants should be able to:”
1. Understand the need to balance oncologic efficacy with functional outcomes in leukoplakia care.
2. Discuss treatment alternatives for laryngeal leukoplakia, emphasizing surgical techniques of KTP, CO2, and cold-instrument phonosurgery in the operating room and pulsed KTP laser treatment in an office setting.
- Head and Neck Surgery and Oncology
Session Introduction
Scott Strome
University of Maryland School of Medicine. USA.
Title: Manipulation of the B7-H1 (PD-L1)-PD-1 Axis for the Treatment of Head and Neck Cancer: A Personal Perspective.

Biography:
Scott Strome, MD, is Professor and Chairman of the Department of Otorhinolaryngology and Interim Chairman of the Department of Dermatology at the University of Maryland School of Medicine. He previously served as Interim Chairman of the Department of Ophthalmology and Visual Sciences and as founder/former leader of the program in tumor immunology and immunotherapy within the Marlene and Stewart Greenebaum Cancer Center. He has contributed nationally as chairman of two NIH special emphasis panels and membership on the Recombinant DNA Advisory Committee. He has excelled in creating drugs and procedures with direct clinical impact. For example, as a Harvard Medical Student, Dr. Strome worked with his father and developed the in vivo models that ultimately resulted in the first human larynx transplant. Similarly, at the Mayo Clinic, Dr. Strome worked with Lieping Chen, MD, to define the translational potential of two costimulatory molecules, B7-H1 (PDL-1) and 4-1BB. The papers resulting from this collaboration are considered seminal works in the field and the intellectual property portfolio on the use of B7-H1, many patents on which Drs. Strome and Chen are named as inventors, has translated into the successful use of these drugs for the treatment of cancer. Finally, Dr. Strome has co-developed a new series of Trojan Peptide Vaccines (TPV) for cancer and evaluated their utility in phase I/II clinical trials. These TPVs, in combination with fully recombinant intravenous immunoglobulin mimetics, serve as core technologies for a biotechnology company, Gliknik Inc., of which Dr. Strome is co-founder. In recognition of these academic-industry initiatives, the University of Maryland Baltimore recognized Dr. Strome as the “2011 Entrepreneur of the Year,” and he was named as Entrepreneur of the year for the University of Maryland in 2013. These scientific endeavors have also resulted in 117 publications in leading basic science and clinical journals.
Abstract:
The ability to block PD-1:PD-L1 interactions has altered our approach to the management of many solid malignancies including head and neck cancer. Despite the success of these therapies, many Otolaryngologists-Head and Neck Surgeons have only limited familiarity with the role of such immuno-oncologic strategies in the management of head and neck cancer. In this talk, Dr. Strome – an inventor of PD-L1 blockade for the treatment of cancer -- will describe some of the original work that identified the PD-1:PD-L1 pathway as a target for cancer therapy, the current role of anti-PD-1/PD-L1 blocking antibodies in the management of head and neck cancer, and potential future directions for manipulating co-signaling pathways for Head and Neck cancer therapy.
Vincent D. Eusterman
Denver Health Medical Center, USA
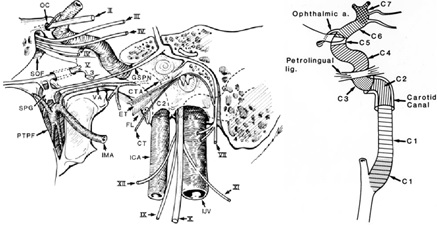
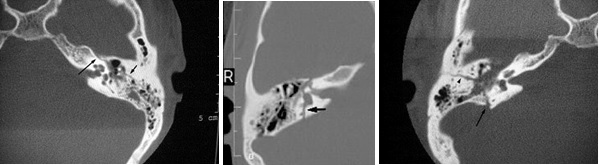
Title: Carotid Artery Injury in Temporal Bone Fractures

Biography:
Biography: Vincent Eusterman, MD, DDS is director of Otolaryngology-Head and Neck Surgery at Denver Health Medical Center and Associate Professor of Surgery in the Department of Otolaryngology-Head and Neck Surgery, University of Colorado School of Medicine. Dr. Eusterman has an extensive background in head and neck trauma, oncologic surgery, and skull base surgery. He is director of the level one trauma hospital division of otolaryngology-head and neck and trauma surgery.
Abstract:
Objective: Temporal bone fractures are commonly evaluated by the otolaryngologist and often extend to numerous cranial structures including the carotid canal. Fracture of the carotid canal can cause carotid injury, hemorrhage, stroke and death. The purpose of this study is to examine the incidence of carotid artery injury in patients who sustain temporal bone fractures to determine the need for carotid injury evaluation.
Methods: We evaluated three databases of clinical, financial and radiographic data from trauma patients treated at our level one trauma center over a 9 year period that met specific criteria for skull base fractures and carotid artery injury. We combined the results from these databases, purging duplicates and cross-referenced our radiology archive and identified 1380 patients with valid radiographic data identifying skull base fractures. The temporal bone radiographs and carotid artery injuries of these patients were then reviewed by two neuroradiologists for accuracy.
Results: Of 1380 skull base fractures, 552 (40%) involved the temporal bone, and 51 (3.69%) involved the carotid artery injury. 34 (2.5%) were neck (C1) injuries, 2 (0.1%) combined C1 and C2-7 injuries, and 15 (1.1%) temporal bone (C2-C7) injuries. When compiling the data 12 patients (2.17%) had both carotid artery and temporal bone fracture.
Discussion: The greatest incidence of carotid artery injury in skull base fractures occurred at the C1 segment from stretch and deformity injury. Temporal bone fractures (C2-C7 segments) had a 2% incidence of carotid injury.
Conclusions: This review of 1380 skull base fractures demonstrated 552 (40%) temporal bone fractures of which 12 (2.17%) patients had associated carotid artery injuries. Otolaryngologists should remain aware of the risk of carotid artery injury with temporal bone fractures and in skull base fractures. The routine use of routine angiography (CTA or 4-vessel angiogram) is probably not necessary in cases of isolated temporal bone fracture.
Produl Hazarika
NMC Specialty Hospital, UAE.
Title: SURGICAL APPROACHES FOR JUVENILE NASOPHARYNGEAL ANGIOFIBROMA –SPECTRUM ANALYSIS

Biography:
Prof Produl Hazarika MBBS, DLO, MS, FACS, FRCS (Edin), FIAO, FUWAI, Fellow of UICC is presently working as an otolaryngologist in NMC Specialty Hospital in Abu Dhabi, U.A.E. He is a former professor and head and director of post graduate studies of the department of Otorhinolaryngology and Head & Neck Surgery in Kasturba Medical College, Manipal, India. He has 28 years of clinical teaching experience both at the undergraduate and postgraduate levels, with over 100 publications in various national and international journals. He was selected as international guest scholar by the American College of Surgeon in 1986 and has travelled widely to the U.S, Australia, U.K and Malaysia, Switzerland, Mauritius on various fellowship programs.
Abstract:
Juvenile nasopharyngeal angiofiboma (JNA) is a very rare benign vascular tumor, occurs, only in adolescent male. 0.5% of all head &neck tumors are JNA. Presenting symptoms of this tumor are profuse, painless, unprovoked, recurrent nasal bleeding. Nasal obstruction in early cases but myriad of symptoms ‘of facial swelling , proptosis and other neurological symptoms may be seen in late cases. JNA though originally arises from nasopharynx also is very much known for its extension to the different parts of the nose, skull base and intracranial spaces, causing both diagnostic and therapeutic problem for the practicing otolaryngologist. Common clinical presentation of these tumors is nasal obstruction in 80 to 90 percent followed by recurrent, painless, profuse and unprovoked epistaxis in 45 to 60 percent of the cases. Radiological investigations included are contrast Ct scan, MRI scan, angiography to find the feeding vessel. Surgical removal of the tumor is the only definitive line of treatment. However, various surgical approaches may be needed depending on its extension and vascular supply. This paper deals with 33 cases of JNA with or without extra nasopharyngeal extension where ten different surgical approaches have been adopted for tumor excision. Logic of application and advantages of surgical procedure in each case of angiofibroma will be highlighted and will be demonstrated in video clip. Newer approaches like endoscopic and Le forte osteotomy will be discussed more in details. Recurrence after surgery, avoidance and treatment will also be discussed.

Biography:
Dr Amith Naragund has completed his Master’s degree in Otorhinolaryngology from Rajiv Gandhi University of Health Sciences, Bengaluru in the year 2007 and Ph.D from KLE University, Belagavi (formerly known as Belgaum) in 2014. After completing his master’s degree, he started working as Assistant Professor and ENT consultant in KLE University’s Jawaharlal Nehru Medical College and KLE hospital, Belagavi. Presently, He is working as Specialist ENT surgeon in UAE (since November 2014).
His research specialization was in the field of Otology (Ossiculoplasty). He has presented papers in National and International conferences and has various publications to his credit. He is also International editorial board member for ‘Otolaryngology International’ journal. The present article has been accepted for publication in the reputed Journal of Laryngology and Otology (U.K).
Abstract:
Objectives: To evaluate the hearing (functional outcome) and graft take up (anatomical outcome) after ossiculoplasty with autograft incus and titanium partial ossicular replacement prosthesis (PORP) in Austin type A ossicular defects and ii) to compare the outcomes of autologous incus interposition ossiculoplasty with titanium PORP
Materials and Methods: This study was conducted on 40 patients in the age group of 10 and 60 years having chronic otitis media with Austin type A ossicular defect who underwent ossiculoplasty. The patients were randomly divided into 2 groups; group A who underwent ossiculoplasty by inter-positioning of autologous incus and group B in whom titanium PORP was used. Otoscopic examination and audiological assessment with conventional pure tone audiometery was done pre and post operatively at 3, 6 and 12 months.
Results: Average post-operative air bone gap (ABG) closure of less than 20 dB was considered as successful hearing gain which was seen in 13 (65%) patients in group A and 07 (35%) in group B.
The average pre-operative ABG value in group A (autologous incus) and group B (PORP) were 42.14+ 6.96 and 44.37+ 9.54 respectively and average post-operative ABG closure after 3 months was 24.23+ 8.50 and 13.05+ 12.46 in group A & B respectively.
The post-operative complications were also much less in group A (20%) as compared to group B (45%). A longer follow up after 6 and 12 months post-operatively did not show any difference in hearing outcome and graft take up.
Conclusion:The hearing results and graft take up rate after ossiculoplasty with autologous incus is significantly better than titanium PORP in reconstruction of Austin A type of ossicular defects. The major disadvantages for the use of titanium PORP is its unpredictable results and higher post-operative complications and extrusion rates as compared to autologous incus.
- Phoniatry and Obstructive sleep apnea(OSA)
Session Introduction
Alessandro Bucci
ENT Department – Senigallia, Italy.
Title: The nose and the OSA (is the evaluation the nose really important in the OSA?): literature review and our personal experience

Biography:
Head of Sleep Apnea Center and Rhinology/Rhino-Allergology Center - Otolaryngology Dept. ASUR Marche – AV2 – Senigallia – Italy. International faculty member of the XXXV Pan-American Congress of Otorhinolaryngology 2016, Cuba. Past Director of the 1st International Conference on Rhinology and Rhino-Allergology / 5th Bulgarian Italian Rhinology Meeting, 2016 Senigallia (Italy). Committee Member and Chairman of the International Specialists Conference on Ear, Nose and Throat Disorders, November 2016 Alicante (Spain). In the past: University Professor at the UNIVPM – Ancona – Italy. International faculty member of the VI Bulgarian Italian Meeting of Rhinology. Dr. Bucci attended medical school at Catholic University (UCSC) in Rome, and completed his residency in Otolaryngology-Head and Neck Surgery at UCSC - Gemelli Hospital in Rome. Reserve Medical Officer of the Italian Navy. Consultant in Otolaryngology from 2002. He has obtained PhD (Rhinology and Rhino-Allergology) in 2006 at UCSC - Rome. Fellowship in Otolaryngology in Spain (University Hospital, Cadiz). Fellowship trained in Facial Plastic Surgery (AMC) and OSAS (Sint Lucas Andreas Hospital) in Amsterdam, The
Netherlands, in Facial Plastic Surgery (Calixto Garcia University Hospital), La Habana, Cuba. Research focused on Rhinology/RhinoAllergology, Sleep Apnea/OSAS, and dysphagia/swallowing disorders. Teaching, management and audit experienced. His other main interest is in humanitarian and international outreach. He is Vice-president of the ONLUS association: “ANATRA.it” (National Association of Tracheotomised patients). Member of the ERS (European Rhinologic Society).
Abstract:
Sleep-disordered breathing (SDB) has been recognized as a serious disorder for a century. The most studied and the most common form of sleep-disordered breathing is OSAS. The nose and pharynx begin the upper airway system and represent a continuum. A biologic basis for nasal obstruction as a cause of SDB lies in the effect of nasal breathing on resistance and flow velocity, which affects the differential pressure between the atmosphere and the intrathoracic space. Nasal airway resistance is responsible for approximately two thirds of the total airway resistance in wakefulness. The nose has been described as a variable resistor with a collapsible segment, such that flow limitation in the nasopharynx results in conditions favorable to downstream pharyngeal collapse. The importance of effectual nasal breathing in maintaining the automatic respiratory rhythms in sleep has long been recognized. An inconsistent link between OSA and nasal obstruction has been reported in the literature for decades but the relationship between obstructive sleep apnea and nasal obstruction is still unclear. The consequences of daily nasal obstruction (allergic rhinitis, chronic sinusitis, septal deviation etc.) on sleep quality have been well demonstrated, resulting poor sleep quality, daytime fatigue and day-to-day discomfort. In order to better understand the relationships between nasal obstruction and OSA, we performed an analysis of the medical literature relating to this subject. According to other authors, we found that when dealing with a patient with sleep apnea, it is not adequate to ascertain the severity of the disease with a sleep test alone; it is imperative to assess the patient’s upper airway and evaluate the airflow dynamics from the nose to the larynx. Our review provides convincing evidence that there is an association between OSA and nasal obstruction.
Helen Caulfield
Royal National Throat, Nose and Ear Hospital. UK.
Title: The use of medical treatment to optimise respiratory function prior to adenotonsillectomy for sleep disordered breathing in the children under 3 years old

Biography:
Helen Caulfield (Nee Myatt) graduated from University College Hospital School of Medicine, London, UK in 1987.Helen showed an early commitment to pursuing a surgical career, obtaining a highly prestigious professorial unit House Officer’s job as her first post at U.C.H. She completed training in Neurosurgery at Kings College and General Surgery at Charing Cross Hospital, London. Subsequently she developed a broad-based ENT training rotating through St.Bartholomew’s Hospital and the North Thames Sector Hospitals, including the prestigious Royal National Throat Nose and Ear Hospital in London and the Radcliffe Infirmary in Oxford. She pursued further training as a Specialist Paediatric ENT Surgeon, by spending two years in Sydney Australia, under the guidance of Bruce Benjamin, a world famous Paediatric Laryngologist. She was a Fellow at the New Children’s Hospital in Sydney during this period. On her return to London in 1999 she took up a post at Great Ormond Street Hospital, and remained there for a 12 month period, prior to obtaining her consultant’s post. In 2000 she was appointed as ENT Consultant at the Royal Free Hospital and Honorary Senior Lecturer at the Royal Free Medical School.
During the last 10 years she has succeeded in raising the profile of the Paediatric ENT Department at the Royal Free Hospital, by providing Paediatric only clinics and operating lists. Her broad knowledge of neonatal ENT has meant she has been able to provide a service for five neonatal units in the North London sector.
Abstract:
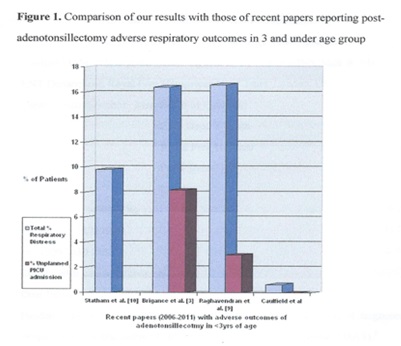
Paediatric sleep disordered breathing encompasses a spectrum ranging from simple snoring to obstructive sleep apnoea syndrome1. Adenotonsillectomy represents an effective treatment for sleep disordered breathing, but the literature reveals that children under 3 years are at greater risk of having more severe obstructive sleep apnoea syndrome and higher rates of postoperative respiratory adverse events2,3. Suddenly relieving the hypercarbia present in some sleep disordered breathing patients by removing the upper airway obstruction can result in pulmonary oedema and acute respiratory failure.
The ENT_UK multidisciplinary working party consensus statement (2008) included children under 2 years (or under 15 kg) with sleep disordered breathing in the ‘at risk’ group. It was recommended that these children should be recovered in intensive care unit facilities5. It was noted that there is currently a lack of evidence for adverse respiratory outcomes in this country with no published case series. We present how we manage the under-3 year age group undergoing adentonsillectomy for sleep disordered breathing in a unit without a paediatric intensive care unit.
- Anesthesia in Ear, Nose and Throat Surgery
Session Introduction
John Greinwald
Cincinnati Children's Hospital Medical Center, USA.
Title: Diagnostic utility of various tests and treatment option for pediatric patients presenting with a unilateral sensorineural hearing loss (SNHL)

Biography:
Dr. John Greinwald is a tenured professor of Otolaryngology and Pediatrics with over 20 years of experience with a focus on the genetic causes and treatment of deafness. Dr. Greinwald co-founded the Ear and Hearing Center at Cincinnati Children’s Hospital Medical Center. He has pioneered the establishment of diagnostic evaluation algorithms for children with sensorineural hearing loss and developed a next generation sequencing platform to determine the genetic causes of hearing loss in children.
He has 81 peer review articles published with the majority related to hearing loss. His research interests concentrate on identifying novel causes of genetic diseases, mitigating barriers to genetic counseling in underserved populations, developing innovative methods of providing complex genetic information to patients and physicians and helped pioneer minimal access cochlear implant surgery. Clinically, he is the Medical Director of the Cochlear Implant Team and faculty in the Auditory Genetics Laboratory of the Ear and Hearing Center.
Dr. Greinwald received his undergraduate B.S. degree from Wofford College and his M.D. degree from the Medical University of South Carolina. His Otolaryngology training was at the Naval Medical Center Portsmouth Virginia and his pediatric otolaryngology fellowship at the University of Iowa. He is board certified in Otolaryngology Head and Neck Surgery
Abstract:
Objective: To determine the diagnostic utility of various tests and treatment option for pediatric patients presenting with a unilateral sensorineural hearing loss (SNHL)
Study Design: Retrospective chart review, uncontrolled case series
Setting: Tertiary academic center; Pediatric Hospital
Subjects: Pediatric patients (<18 years old) evaluated for unilateral SNHL
Methods: Upon IRB approval patients with single sided SNHL were identified using an internal database. Audiologic data, genetic testing, imaging results and pertinent clinical information were analyzed to determine the most efficacious method of evaluating these patients.
Results: 407 patients were identified with average age (SD) of 87.4 months (53.9). 233 patients were males (53%). 37 patients had high frequency (HF) SNHL alone, 51 patients with normal HF PTA (abnormal low frequency PTA) and 319 with a flat audiometric configuration. Hearing loss was more common on the left side and in males. More than 50% of patients had mild to moderate SNHL. GJB2 was a rarely seen (0.7%), while mutations in the SLC26A4 gene were seen in 18% of patients. Enlarged vestibular aqueduct (EVA) was found in 17% of patients. In patients with unilateral EVA, 19% had contralateral ear involvement. Overall, 19% of patients developed bilateral hearing loss. Treatments varied from observation, traditional hearing aids, CROS hearing aids and cochlear implantation. Seven patients with single sided deafness were implanted. All patients continue wearing their implants and getting appropriate aided benefit with speech reception thresholds at 30dB or better with a minimum of 2 years of follow up.
Conclusion: USNHL is a relatively common problem affecting children. In our population, progression occurred relatively frequently. Temporal bone anomalies such as EVA, were common. Cochlear nerve deficiencies are also demonstrated in our study and are best demonstrated on MRI. Pendred syndrome and DFNB1 are rare. Based on our data, an algorithm for children with USNHL shows that imaging should be the primary diagnostic study. Magnetic resonance imaging may be the best imaging modality due to its ability to diagnose deficient cochlear nerves in addition to common temporal bone anomalies. Treatment should be individualized based on the medical needs of the child. Cochlear implantation is now an option for patients with single sided deafness.
Kurt J. Knowles
Louisiana State University, USA.
Title: Oral foregut duplication cysts: A rare and fascinating congenital lesion Case report

Biography:
Dr. Knowles completed a Pathology residency from 1991-1996 then completed a cytopathology fellowship from 1996-1997. He was in private practice from 1997 to 2015 but has recently transitioned from 18 years in private practice in pathology and returned to the medical center practice of pathology at Louisiana State Health Science Center in Shreveport LA. His responsibilities include teaching medical students and pathology residents, and pathology to internal medicine residents. His subspecialty sign-out responsibilities include cytopathology, gastrointestinal pathology and head and neck pathology. The faculty at LSU are engaged in numerous research activities covering many areas of clinical and academic medicine. The article presented at this meeting combines gastroenterology pathology; head and neck pathology with implications for developmental pediatrics, OB-Gyn, anesthesia and embryology.
Abstract:
Oral foregut duplication cysts are extremely rare lesions with approximately 57 cases reported. They are congenital cysts, located in the anterior or ventral tongue, and occur predominantly in males. They are lined by one or more types of epithelia which is limited to gastric, intestinal or respiratory epithelium. The differential diagnosis includes lymphangioma, hemangioma, ranula, epidermoid cyst, teratoma and less likely a malignant process. They are congenital and if present at birth or early infancy, and they can cause difficulties in feeding, swallowing, speech, and airway obstruction. If discovered in utero and suspected to be large enough, they may also cause respiratory distress and optimal patient care would dictate that ENT be present at delivery. Even a small lesion if left untreated may cause speech difficulties in toddlers so definitive treatment is required.
What is fascinating about oral foregut duplication cysts is the possible histogenesis. They are always comprised of one or more upper GI and/or respiratory tissues. This trapped primitive tissue, apparently removed from its normal milieu, still has the capability to differentiate into gastric, intestinal or respiratory tissue, singly or in combinations of epithelia as was this case. This suggests that the trapped cells are preprogrammed to differentiate along certain possible cell lines but are influenced by some unknown local or distant environmental factors.
Jerome Thompson
University of Tennessee Health Science Center, USA.
Title: The EXIT Procedure: Current Status and Technical Tips for Otolaryngologist

Biography:
Dr. Jerome Thompson is an ENT-otolaryngologist in Memphis, Tennessee and is affiliated with multiple hospitals in the area, including Baptist Memorial Hospital-Memphis and Memphis Veterans Affairs Medical Center. He received his medical degree from David Geffen School of Medicine at UCLA and has been in practice for more than 20 years. Dr. Thompson accepts several types of health insurance, listed below. He is one of 35 doctors at Baptist Memorial Hospital-Memphis and one of 5 at Memphis Veterans Affairs Medical Center who specialize in Otolaryngology.
Abstract:
Prior to the 1980s, births of fetuses with congenital abnormalities causing airway obstruction had mortality rates approaching 40%. Anoxic brain injury results if the airway is not secured within 5 minutes following termination of maternal-fetal circulation. The advent of the EXIT (ex utero intrapartum therapy) procedure allowed surgeons to operate on a partially delivered fetus, still connected to maternal circulation. This significantly extending the time allowed to secure the airway. It is particularly useful in cases of Congenital High Airway Obstruction Syndrome or CHAOS. Pediatric otolaryngologists have used the EXIT since 1994. It remains an infrequently performed operation, with even the largest academic pediatric hospitals averaging approximately only 5 procedures per year. It is now part of the armamentarium of pediatric and cardiovascular surgeons. In this article, we share our 9 most interesting experiences with the EXIT procedure, and what we have learned from each case.
Amjad Alnuseirat
Jordan University of Science and Technology, Jordan
Title: Using 3D technology for functional and cosmetic solution in patients with microtia

Biography:
Assistant professor at Jordan University of Science and Technology, Otolaryngologist at King Abdullah University Hospital. After finishing medical degree, joined residency program in otolaryngology. Got my fellowship degree in otology and skull base surgery from Italy.
After returning to Jordan joined teaching of medical students and ENT residents in JUST/KAUH. I am otolaryngologist mainly interested in otology. I am trained to do otologic surgeries mainly concentrating on cochlear implants and prosthetic ear implants. I have published a number of articles in highly ranked medical journals.
Abstract:
Microtia is a congenital malformation of variable severity of the external ear affecting external ear (with or without middle ear) components shape and position. This deformity affects 3 of every 10,000 live births. In 10% of cases could be bilateral.
Microtia may present within a spectrum of branchial arch defects (hemifacial microsomia, craniofacial microsomia) or may manifest as an independent malformation.
Hearing loss and cosmetic discomfort may affect child scholastic performance and leads to social withdrawal.
Reconstruction of shape and hearing acuity is a challenge even for experienced surgeons. The prosthetic ear is aesthetically pleasing, composed of natural looking anatomical contours, shape, and texture along with good color that blends with surrounding existing skin. Bone anchoring hearing aids (BAHA) is one of the most affective hearing solutions. Combining of the BAHA implant and prosthetic ear attached by titanium screws may give both functional and psychological relief for both child and parents. These outcomes can be optimized by the integration of digital technologies in the construction process. CT scan images in cases of uni or bilateral cases can be processed in special software to give a mirror image of the present contralateral ear or ideal position for implant insertion in bilateral cases. Giving clear idea about bone quality and best insertion site of vistafix prosthetic ear and BAHA implants.
Using specialized 3D printers can give us ideal shaped prosthetic ear which can be colored according to patient specific skin color providing a base for reproducible results regardless of operator.
This modality of treatment can give us pleasant safe solution for function and cosmetic appearance.
- Phoniatry and Obstructive sleep apnea(OSA)
Session Introduction
Alessandro Bucci
ENT Department – Senigallia, Italy
Title: Endoscopic evaluation of airway obstruction during sleep in OSAS: an update on recent literature and our personal experience

Biography:
Head of Sleep Apnea Center and Rhinology/Rhino-Allergology Center - Otolaryngology Dept. ASUR Marche – AV2 – Senigallia – Italy. International faculty member of the XXXV Pan-American Congress of Otorhinolaryngology 2016, Cuba. Past Director of the 1st International Conference on Rhinology and Rhino-Allergology / 5th Bulgarian Italian Rhinology Meeting, 2016 Senigallia (Italy). Committee Member and Chairman of the International Specialists Conference on Ear, Nose and Throat Disorders, November 2016 Alicante (Spain). In the past: University Professor at the UNIVPM – Ancona – Italy.
International faculty member of the VI Bulgarian Italian Meeting of Rhinology. Dr. Bucci attended medical school at Catholic University (UCSC) in Rome, and completed his residency in Otolaryngology-Head and Neck Surgery at UCSC - Gemelli Hospital in Rome. Reserve Medical Officer of the Italian Navy. Consultant in Otolaryngology from 2002. PhD (Rhinology and Rhino-Allergology) in 2006 at UCSC - Rome. Fellowship in Otolaryngology in Spain (University Hospital, Cadiz). Fellowship trained in Facial Plastic Surgery (AMC) and OSAS (Sint Lucas Andreas Hospital) in Amsterdam, The Netherlands, in Facial Plastic Surgery (Calixto Garcia University Hospital), La Habana, Cuba. Research focused on Rhinology/RhinoAllergology, Sleep Apnea/OSAS, and dysphagia/swallowing disorders. Teaching, management and audit experienced. His other main interest is in humanitarian and international outreach. He is Vice-president of the ONLUS association: “ANATRA.it” (National Association of Tracheotomised patients). Member of the ERS (European Rhinologic Society).
Abstract:
Obstructive sleep apnea (OSA) is a sleep disorder that involves cessation or significant decrease in airflow in the presence of breathing effort. Airway obstruction in OSA may occur at many levels. Surgical procedures are inherently directed at specific regions of the upper airway. Traditionally, upper airway examination is performed while the patient is awake. Nasofibrolaryngoscopy under induced sleep is a promising alternative for identifying sites of upper airway obstruction in patients with OSA. The purpose of this study was to systematically review the evidence regarding the usefulness of Drug Induced Sleep Endoscopy (DISE) compared with that of traditional awake examination for surgical decision-making in patients with OSAS. This review emphasizes the direct impact of DISE compared with that of awake examination on surgical decision-making in OSA patients.
Materials and methods. We performed a systematic review of studies using DISE to identify obstruction sites and patterns of obstruction in patients with OSA. Only studies with a primary objective of evaluating the usefulness of DISE for surgical decision-making and the importance of identifying multilevel obstruction were selected. Then a retrospective chart review of OSAS patients who underwent DISE at our Centre for Diagnosis and Treatment of Respiratory Sleep Disorders, as part of their surgical evaluation, were reviewed. According to others authors we found that palatal obstruction was the most frequently observed site of obstruction, followed by tongue base obstruction, laryngeal obstruction and hypopharyngeal obstruction.
Conclusion. Although consensus has been reached on several aspects of the DISE procedure some topics remain open to future research. DISE is an additional method to reveal obstruction sites that have not been detected in awake patients. DISE is mandatory in the diagnostic work-up of OSA and is a valid addition when surgery is considered. Anyway, larger detailed analyses are needed to determine the importance of each site and degree of obstruction seen on DISE.
- poster presentations
Session Introduction
Jeong Mi Park
Gwangju Veterans Hospital, South Korea.
Title: Responses from a Supplemental Question used in Otolaryngology Residency Applications

Biography:
Abstract:
Objective: 1) To categorize and analyze applicant responses to a supplemental question used during the applicant selection process. 2) To assess the incidence of leadership training as an element in applicant response over three match cycles
Study Design: Qualitative retrospective review of applicant responses to a supplemental question during the 2012, 2013, and 2014 match cycles. Setting: Academic otolaryngology residency training program.
Subjects and Methods: Responses to a supplemental question were analyzed and specific elements were categorized. Frequency of each reason was assessed by match cycle and gender. Chi square test was performed on proportion of responses containing leadership related elements by year and gender. Statistical significance was defined as p-value <0.05.
Results: Of the 592 responses that were analyzed, 394 were males and 194 were females. 3 applicants' gender could not be identified with available ERAS data. The most often cited reasons for applying were research opportunities (69%), education and training (57%), leadership program (48%), comprehensiveness of subspecialties (36%), reputation (25%), and location (17%). There was a statistically significant difference in the proportion of leadership program in each of the three years (p≤0.01).
Conclusions: We describe the use of a supplemental application question during the residency match cycle designed to help select applicants for interview that would best “fit” with our program focused on leadership. We hope this will stimulate consideration of how to improve the “fit” of applicants to otolaryngology residency programs.
Aseel Almeqbel
Kuwait University, Kuwait
Title: Temporal Encoding of Voice Onset Time in Young Children

Biography:
Academic position: Assistance Professor of Audiology in the Department of Hearing and Speech Sciences, Health Science Center (HSC), Faculty of the Allied Health Sciences, Kuwait university. Audiology Program Coordinator.Degree Holding: B.Sc. Audiology, M.Sc. Clinical Audiology, Ph.D. Academic Doctorates of Audiology Member of Audiology Society of Australia (MASA) Certificate of Clinical-Competence (CCC-A) -Audiology Clinical work: Pediatric Audiology Consultant
Research interest: Pediatric Audiology, Educational Audiology, auditory physiology and electrophysiology (objective measures in infant and young children) , Hearing in children with cancer, Cochlear Implantation in Auditory Neuropathy Spectrum Disorder, Clinical Audiology, Cortical auditory evoked potential in infants and young children, hearing screening (newborn and school aged children) and cochlear implant in pediatric population.
Abstract:
Objective: Voice onset time (VOT) is an important parameter of speech that denotes the time interval between consonant onset and the onset of low frequency periodicity generated. In this study we examined the temporal encoding of voice onset time in the cortical auditory evoked response (CAEP) of young children.
Methods: Scalp recoded CAEP were measured in 18 children aged from 5-8 participated (n=18). The N2 latency was evoked using differences in voice-onset-times (VOTs) using stop consonant-vowel syllables /ga/-/ka/.
Results: A significant and systematic shift in the N2 latency was observed for differences in VOT.
Conclusions: Our results demonstrate that temporal encoding of VOT exists in the developing cortical evoked response.
