Day 2 :
- Head and Neck Surgery and Oncology
Session Introduction
Scott Strome
University of Maryland School of Medicine. USA.
Title: Manipulation of the B7-H1 (PD-L1)-PD-1 Axis for the Treatment of Head and Neck Cancer: A Personal Perspective.

Biography:
Scott Strome, MD, is Professor and Chairman of the Department of Otorhinolaryngology and Interim Chairman of the Department of Dermatology at the University of Maryland School of Medicine. He previously served as Interim Chairman of the Department of Ophthalmology and Visual Sciences and as founder/former leader of the program in tumor immunology and immunotherapy within the Marlene and Stewart Greenebaum Cancer Center. He has contributed nationally as chairman of two NIH special emphasis panels and membership on the Recombinant DNA Advisory Committee. He has excelled in creating drugs and procedures with direct clinical impact. For example, as a Harvard Medical Student, Dr. Strome worked with his father and developed the in vivo models that ultimately resulted in the first human larynx transplant. Similarly, at the Mayo Clinic, Dr. Strome worked with Lieping Chen, MD, to define the translational potential of two costimulatory molecules, B7-H1 (PDL-1) and 4-1BB. The papers resulting from this collaboration are considered seminal works in the field and the intellectual property portfolio on the use of B7-H1, many patents on which Drs. Strome and Chen are named as inventors, has translated into the successful use of these drugs for the treatment of cancer. Finally, Dr. Strome has co-developed a new series of Trojan Peptide Vaccines (TPV) for cancer and evaluated their utility in phase I/II clinical trials. These TPVs, in combination with fully recombinant intravenous immunoglobulin mimetics, serve as core technologies for a biotechnology company, Gliknik Inc., of which Dr. Strome is co-founder. In recognition of these academic-industry initiatives, the University of Maryland Baltimore recognized Dr. Strome as the “2011 Entrepreneur of the Year,” and he was named as Entrepreneur of the year for the University of Maryland in 2013. These scientific endeavors have also resulted in 117 publications in leading basic science and clinical journals.
Abstract:
The ability to block PD-1:PD-L1 interactions has altered our approach to the management of many solid malignancies including head and neck cancer. Despite the success of these therapies, many Otolaryngologists-Head and Neck Surgeons have only limited familiarity with the role of such immuno-oncologic strategies in the management of head and neck cancer. In this talk, Dr. Strome – an inventor of PD-L1 blockade for the treatment of cancer -- will describe some of the original work that identified the PD-1:PD-L1 pathway as a target for cancer therapy, the current role of anti-PD-1/PD-L1 blocking antibodies in the management of head and neck cancer, and potential future directions for manipulating co-signaling pathways for Head and Neck cancer therapy.
Vincent D. Eusterman
Denver Health Medical Center, USA
Title: Carotid Artery Injury in Temporal Bone Fractures

Biography:
Biography: Vincent Eusterman, MD, DDS is director of Otolaryngology-Head and Neck Surgery at Denver Health Medical Center and Associate Professor of Surgery in the Department of Otolaryngology-Head and Neck Surgery, University of Colorado School of Medicine. Dr. Eusterman has an extensive background in head and neck trauma, oncologic surgery, and skull base surgery. He is director of the level one trauma hospital division of otolaryngology-head and neck and trauma surgery.
Abstract:
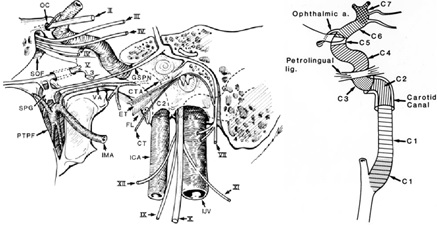
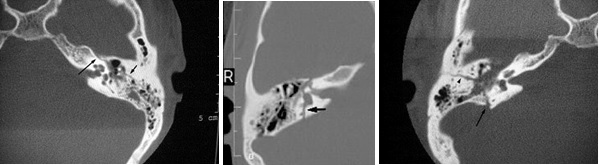
Objective: Temporal bone fractures are commonly evaluated by the otolaryngologist and often extend to numerous cranial structures including the carotid canal. Fracture of the carotid canal can cause carotid injury, hemorrhage, stroke and death. The purpose of this study is to examine the incidence of carotid artery injury in patients who sustain temporal bone fractures to determine the need for carotid injury evaluation.
Methods: We evaluated three databases of clinical, financial and radiographic data from trauma patients treated at our level one trauma center over a 9 year period that met specific criteria for skull base fractures and carotid artery injury. We combined the results from these databases, purging duplicates and cross-referenced our radiology archive and identified 1380 patients with valid radiographic data identifying skull base fractures. The temporal bone radiographs and carotid artery injuries of these patients were then reviewed by two neuroradiologists for accuracy.
Results: Of 1380 skull base fractures, 552 (40%) involved the temporal bone, and 51 (3.69%) involved the carotid artery injury. 34 (2.5%) were neck (C1) injuries, 2 (0.1%) combined C1 and C2-7 injuries, and 15 (1.1%) temporal bone (C2-C7) injuries. When compiling the data 12 patients (2.17%) had both carotid artery and temporal bone fracture.
Discussion: The greatest incidence of carotid artery injury in skull base fractures occurred at the C1 segment from stretch and deformity injury. Temporal bone fractures (C2-C7 segments) had a 2% incidence of carotid injury.
Conclusions: This review of 1380 skull base fractures demonstrated 552 (40%) temporal bone fractures of which 12 (2.17%) patients had associated carotid artery injuries. Otolaryngologists should remain aware of the risk of carotid artery injury with temporal bone fractures and in skull base fractures. The routine use of routine angiography (CTA or 4-vessel angiogram) is probably not necessary in cases of isolated temporal bone fracture.
Produl Hazarika
NMC Specialty Hospital, UAE.
Title: SURGICAL APPROACHES FOR JUVENILE NASOPHARYNGEAL ANGIOFIBROMA –SPECTRUM ANALYSIS

Biography:
Prof Produl Hazarika MBBS, DLO, MS, FACS, FRCS (Edin), FIAO, FUWAI, Fellow of UICC is presently working as an otolaryngologist in NMC Specialty Hospital in Abu Dhabi, U.A.E. He is a former professor and head and director of post graduate studies of the department of Otorhinolaryngology and Head & Neck Surgery in Kasturba Medical College, Manipal, India. He has 28 years of clinical teaching experience both at the undergraduate and postgraduate levels, with over 100 publications in various national and international journals. He was selected as international guest scholar by the American College of Surgeon in 1986 and has travelled widely to the U.S, Australia, U.K and Malaysia, Switzerland, Mauritius on various fellowship programs.
Abstract:
Juvenile nasopharyngeal angiofiboma (JNA) is a very rare benign vascular tumor, occurs, only in adolescent male. 0.5% of all head &neck tumors are JNA. Presenting symptoms of this tumor are profuse, painless, unprovoked, recurrent nasal bleeding. Nasal obstruction in early cases but myriad of symptoms ‘of facial swelling , proptosis and other neurological symptoms may be seen in late cases. JNA though originally arises from nasopharynx also is very much known for its extension to the different parts of the nose, skull base and intracranial spaces, causing both diagnostic and therapeutic problem for the practicing otolaryngologist. Common clinical presentation of these tumors is nasal obstruction in 80 to 90 percent followed by recurrent, painless, profuse and unprovoked epistaxis in 45 to 60 percent of the cases. Radiological investigations included are contrast Ct scan, MRI scan, angiography to find the feeding vessel. Surgical removal of the tumor is the only definitive line of treatment. However, various surgical approaches may be needed depending on its extension and vascular supply. This paper deals with 33 cases of JNA with or without extra nasopharyngeal extension where ten different surgical approaches have been adopted for tumor excision. Logic of application and advantages of surgical procedure in each case of angiofibroma will be highlighted and will be demonstrated in video clip. Newer approaches like endoscopic and Le forte osteotomy will be discussed more in details. Recurrence after surgery, avoidance and treatment will also be discussed.

Biography:
Dr Amith Naragund has completed his Master’s degree in Otorhinolaryngology from Rajiv Gandhi University of Health Sciences, Bengaluru in the year 2007 and Ph.D from KLE University, Belagavi (formerly known as Belgaum) in 2014. After completing his master’s degree, he started working as Assistant Professor and ENT consultant in KLE University’s Jawaharlal Nehru Medical College and KLE hospital, Belagavi. Presently, He is working as Specialist ENT surgeon in UAE (since November 2014).
His research specialization was in the field of Otology (Ossiculoplasty). He has presented papers in National and International conferences and has various publications to his credit. He is also International editorial board member for ‘Otolaryngology International’ journal. The present article has been accepted for publication in the reputed Journal of Laryngology and Otology (U.K).
Abstract:
Objectives: To evaluate the hearing (functional outcome) and graft take up (anatomical outcome) after ossiculoplasty with autograft incus and titanium partial ossicular replacement prosthesis (PORP) in Austin type A ossicular defects and ii) to compare the outcomes of autologous incus interposition ossiculoplasty with titanium PORP
Materials and Methods: This study was conducted on 40 patients in the age group of 10 and 60 years having chronic otitis media with Austin type A ossicular defect who underwent ossiculoplasty. The patients were randomly divided into 2 groups; group A who underwent ossiculoplasty by inter-positioning of autologous incus and group B in whom titanium PORP was used. Otoscopic examination and audiological assessment with conventional pure tone audiometery was done pre and post operatively at 3, 6 and 12 months.
Results: Average post-operative air bone gap (ABG) closure of less than 20 dB was considered as successful hearing gain which was seen in 13 (65%) patients in group A and 07 (35%) in group B.
The average pre-operative ABG value in group A (autologous incus) and group B (PORP) were 42.14+ 6.96 and 44.37+ 9.54 respectively and average post-operative ABG closure after 3 months was 24.23+ 8.50 and 13.05+ 12.46 in group A & B respectively.
The post-operative complications were also much less in group A (20%) as compared to group B (45%). A longer follow up after 6 and 12 months post-operatively did not show any difference in hearing outcome and graft take up.
Conclusion:The hearing results and graft take up rate after ossiculoplasty with autologous incus is significantly better than titanium PORP in reconstruction of Austin A type of ossicular defects. The major disadvantages for the use of titanium PORP is its unpredictable results and higher post-operative complications and extrusion rates as compared to autologous incus.
- Phoniatry and Obstructive sleep apnea(OSA)
Session Introduction
Alessandro Bucci
ENT Department – Senigallia, Italy.
Title: The nose and the OSA (is the evaluation the nose really important in the OSA?): literature review and our personal experience

Biography:
Head of Sleep Apnea Center and Rhinology/Rhino-Allergology Center - Otolaryngology Dept. ASUR Marche – AV2 – Senigallia – Italy. International faculty member of the XXXV Pan-American Congress of Otorhinolaryngology 2016, Cuba. Past Director of the 1st International Conference on Rhinology and Rhino-Allergology / 5th Bulgarian Italian Rhinology Meeting, 2016 Senigallia (Italy). Committee Member and Chairman of the International Specialists Conference on Ear, Nose and Throat Disorders, November 2016 Alicante (Spain). In the past: University Professor at the UNIVPM – Ancona – Italy. International faculty member of the VI Bulgarian Italian Meeting of Rhinology. Dr. Bucci attended medical school at Catholic University (UCSC) in Rome, and completed his residency in Otolaryngology-Head and Neck Surgery at UCSC - Gemelli Hospital in Rome. Reserve Medical Officer of the Italian Navy. Consultant in Otolaryngology from 2002. He has obtained PhD (Rhinology and Rhino-Allergology) in 2006 at UCSC - Rome. Fellowship in Otolaryngology in Spain (University Hospital, Cadiz). Fellowship trained in Facial Plastic Surgery (AMC) and OSAS (Sint Lucas Andreas Hospital) in Amsterdam, The
Netherlands, in Facial Plastic Surgery (Calixto Garcia University Hospital), La Habana, Cuba. Research focused on Rhinology/RhinoAllergology, Sleep Apnea/OSAS, and dysphagia/swallowing disorders. Teaching, management and audit experienced. His other main interest is in humanitarian and international outreach. He is Vice-president of the ONLUS association: “ANATRA.it” (National Association of Tracheotomised patients). Member of the ERS (European Rhinologic Society).
Abstract:
Sleep-disordered breathing (SDB) has been recognized as a serious disorder for a century. The most studied and the most common form of sleep-disordered breathing is OSAS. The nose and pharynx begin the upper airway system and represent a continuum. A biologic basis for nasal obstruction as a cause of SDB lies in the effect of nasal breathing on resistance and flow velocity, which affects the differential pressure between the atmosphere and the intrathoracic space. Nasal airway resistance is responsible for approximately two thirds of the total airway resistance in wakefulness. The nose has been described as a variable resistor with a collapsible segment, such that flow limitation in the nasopharynx results in conditions favorable to downstream pharyngeal collapse. The importance of effectual nasal breathing in maintaining the automatic respiratory rhythms in sleep has long been recognized. An inconsistent link between OSA and nasal obstruction has been reported in the literature for decades but the relationship between obstructive sleep apnea and nasal obstruction is still unclear. The consequences of daily nasal obstruction (allergic rhinitis, chronic sinusitis, septal deviation etc.) on sleep quality have been well demonstrated, resulting poor sleep quality, daytime fatigue and day-to-day discomfort. In order to better understand the relationships between nasal obstruction and OSA, we performed an analysis of the medical literature relating to this subject. According to other authors, we found that when dealing with a patient with sleep apnea, it is not adequate to ascertain the severity of the disease with a sleep test alone; it is imperative to assess the patient’s upper airway and evaluate the airflow dynamics from the nose to the larynx. Our review provides convincing evidence that there is an association between OSA and nasal obstruction.
Helen Caulfield
Royal National Throat, Nose and Ear Hospital. UK.
Title: The use of medical treatment to optimise respiratory function prior to adenotonsillectomy for sleep disordered breathing in the children under 3 years old

Biography:
Helen Caulfield (Nee Myatt) graduated from University College Hospital School of Medicine, London, UK in 1987.Helen showed an early commitment to pursuing a surgical career, obtaining a highly prestigious professorial unit House Officer’s job as her first post at U.C.H. She completed training in Neurosurgery at Kings College and General Surgery at Charing Cross Hospital, London. Subsequently she developed a broad-based ENT training rotating through St.Bartholomew’s Hospital and the North Thames Sector Hospitals, including the prestigious Royal National Throat Nose and Ear Hospital in London and the Radcliffe Infirmary in Oxford. She pursued further training as a Specialist Paediatric ENT Surgeon, by spending two years in Sydney Australia, under the guidance of Bruce Benjamin, a world famous Paediatric Laryngologist. She was a Fellow at the New Children’s Hospital in Sydney during this period. On her return to London in 1999 she took up a post at Great Ormond Street Hospital, and remained there for a 12 month period, prior to obtaining her consultant’s post. In 2000 she was appointed as ENT Consultant at the Royal Free Hospital and Honorary Senior Lecturer at the Royal Free Medical School.
During the last 10 years she has succeeded in raising the profile of the Paediatric ENT Department at the Royal Free Hospital, by providing Paediatric only clinics and operating lists. Her broad knowledge of neonatal ENT has meant she has been able to provide a service for five neonatal units in the North London sector.
Abstract:
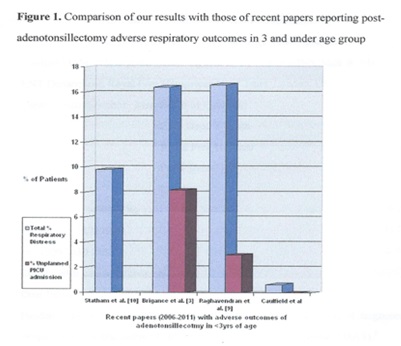
Paediatric sleep disordered breathing encompasses a spectrum ranging from simple snoring to obstructive sleep apnoea syndrome1. Adenotonsillectomy represents an effective treatment for sleep disordered breathing, but the literature reveals that children under 3 years are at greater risk of having more severe obstructive sleep apnoea syndrome and higher rates of postoperative respiratory adverse events2,3. Suddenly relieving the hypercarbia present in some sleep disordered breathing patients by removing the upper airway obstruction can result in pulmonary oedema and acute respiratory failure.
The ENT_UK multidisciplinary working party consensus statement (2008) included children under 2 years (or under 15 kg) with sleep disordered breathing in the ‘at risk’ group. It was recommended that these children should be recovered in intensive care unit facilities5. It was noted that there is currently a lack of evidence for adverse respiratory outcomes in this country with no published case series. We present how we manage the under-3 year age group undergoing adentonsillectomy for sleep disordered breathing in a unit without a paediatric intensive care unit.