Day 1 :
- Laryngology

Chair
Lee Akst
Johns Hopkins University
Session Introduction
Lee Akst
Johns Hopkins University, USA.
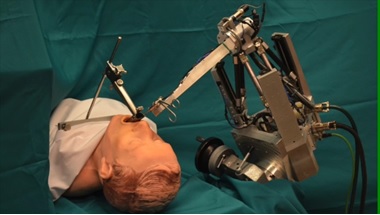
Title: Evolutions in Robotic Microlaryngeal Surgery

Biography:
Dr. Lee Akst is head of the Johns Hopkins Voice Center and is Director of the Division of Laryngology at the Johns Hopkins University Department of Otolaryngology-Head and Neck Surgery. The focus of his clinical practice is on management of voice disorders, with focus on office-based treatments and operative management of epithelial diseases such as vocal cord leukoplakia, papilloma, and early glottis cancer. He has lectured extensively on phonosurgical techniques, treatment of laryngeal leukoplakia, laryngopharyngeal reflux, and globus pharyngeus. He has been working with engineers at Johns Hopkins on novel robotic platforms to bringing robotic surgery into the endolarynx to aid microlaryngeal operative precision. Dr. Akst received his undergraduate and medical degrees from Yale University, did his Otolaryngology residency at the Cleveland Clinic, and completed his laryngology fellowship at Massachusetts General Hospital.
Abstract:
This presentation will review limitations of current robotic approaches to microlaryngoscopy, and will introduce the audience to a new robotic technology with the potential to change how microlaryngeal surgeries are performed. The evolution of laryngeal surgical techniques have been driven by the promise of increased operative precision. Coincident with advances in microlaryngeal surgery have been similar, though more rapid, advances in robot-assisted surgery within Otolaryngology. From well-established use of the da Vinci surgical robot for ablative procedures of the pharynx to newer applications for robot-assisted procedures such as thyroid surgery and skull base surgery, robotic-assisted surgery is growing.
Despite these advances, robot-assisted surgery is not yet routinely incorporated into microlaryngeal surgery. Current limitations for existing commercial systems include size of available instrumentation, difficulty manipulating robotic effector arms within narrow working space afforded by standard retractors, and reduced haptic feedback that comes from working remotely rather than handling tissues directly. Even as smaller instruments and new retractors are being developed, existing robots have been largely limited to laryngeal procedures such as vocal cord stripping, cordectomy, and partial epiglottectomy – procedures in which preservation of normal vocal fold anatomy and function are not prioritized.
To address these issues and create a role for robotic assistance in microlaryngoscopy, a novel robotic ENT microsurgery system (REMS) has been developed. This system emphasizes cooperative control, rather than remote control, of a microsurgical instrument; traditional microlaryngoscopy instruments are utilized with both the robot arm and surgeon controlling the same instrument. The ability of this REMS system to improve precise performance of simulated microlaryngoscopy tasks has been demonstrated in a variety of research studies. These preliminary studies, their methods, and their results will be reviewed; surgical videos will demonstrate the robot ‘in action’. The REMS platform may represent the next step in the evolution of robotic microlaryngeal surgery.
Alessandro Bucci
ENT Department – Senigallia, Italy
Title: Endoscopic evaluation during sleep of airway obstruction in OSAS: an update on recent literature and our personal in experience

Biography:
Alessandro Bucci is a Reserve Medical Officer of Italian Navy. He has Fellowship experienced in Otolaryngology at University Hospital, Cadiz, Spain. He was a Consultant in Otolaryngology. He has Fellowship in Facial Plastic Surgery (AMC) and OSAS at Sint Lucas Andreas Hospital, Amsterdam, Netherlands and in Facial Plastic Surgery at C. Garcia University Hospital, Cuba. He is a dedicated ENT Specialist Surgeon with 14 years of experience providing the highest standard of treatment. His research focused on rhinology/rhinoallergology, OSAS and dysphagia.
Abstract:
Obstructive sleep apnea (OSA) is a sleep disorder that involves cessation or significant decrease in airflow in the presence of breathing effort. Airway obstruction in OSA can occur at many levels. Surgical procedures are inherently directed at specific regions of the upper airway. Traditionally, upper airway examination is performed while the patient is awake. Nasofibrolaryngoscopy under induced sleep is a promising alternative for identifying sites of upper airway obstruction in patients with OSA. The purpose of this study was to systematically review the evidence regarding the usefulness of Drug Induced Sleep Endoscopy (DISE) compared with that of traditional awake examination for surgical decision- making in patients with OSAS. This review emphasized the direct impact of DISE compared with that of awake examination on surgical decision-making in OSA patients.
Materials and methods used. DISE has been used as a method of evaluation of the upper airway during pharmacologically induced sleep. During DISE artificial sleep is induced by propofol, and the pharyngeal collapse patterns are visualized using a flexible fiberoptic nasopharyngoscope. A systematic review was performed of studies using DISE to identify obstruction sites and patterns of obstruction in patients with OSA. The level (palate, oropharynx, tongue base, hypopharynx/epiglottis), the direction (antero-posterior, concentric, lateral), and the degree of collapse were scored according to the NOHL classification. Only studies with a primary objective of evaluating the usefulness of DISE for surgical decision-making and the importance of identifying multilevel obstruction were selected. Then a retrospective chart review of OSAS patients who underwent DISE at our Centre for Diagnosis and Treatment of Respiratory Sleep Disorders, as part of their surgical evaluation, were reviewed. We compared the results of clinical and diagnostic evaluation with those of sleep endoscopy. According to others authors we found that palatal obstruction was the most frequently observed site of obstruction, followed by tongue base obstruction, laryngeal obstruction and hypopharyngeal obstruction.
Conclusion. Although consensus has been reached on several aspects of the DISE procedure some topics remain open to future research. DISE is an additional method to reveal obstruction sites that have not been detected in awake patients. DISE is mandatory in the diagnostic work-up of OSA and is a valid addition when surgery is considered. DISE is a dynamic, safe, and easy-to-perform technique that visualizes the anatomical sites of snoring or apnoeas. Anyway, larger detailed analyses are needed to determine the importance of each site and degree of obstruction seen on DISE.
Zeyad mandour
Alexandria University, EGYPT.
Title: To evaluate endoscopic closure of nasal septal perforation using pedicled inferior turbinate flap

Biography:
Oto-rhino-laryngology and Head & Neck Surgery M.D -Consultant of Endoscopic Sinus Surgery & Microscopic Ear Surgery -ORL Professor, Alexandria University -- Fellowship Marseilles- France.
Abstract:
Septal perforations are usually difficult to treat. Surgery is indicated if the perforation is symptomatic. Our aim is to evaluate endoscopic closure of nasal septal perforation using pedicled inferior turbinate flap.
Patients and Methods: Endoscopic closure of nasal septum perforations were performed in 31 patients using unilateral pedicled inferior turbinate flap.
Results: Twenty-three patients (74%) had complete closure of their perforations. Six other patients (19.5%) had incomplete closure with a small residual perforation< 1cm in diameter posteriorly. Two patients (6.5%), who had previous submucosal diathermy of the inferior turbinate, had flap necrosis with complete failure of the repair. There was a significant inverse relationship between the diameter of the perforation and the success of the repair.
Conclusions: Endoscopic repair of nasal septal perforations, up to 2 cm in diameter, using a modified pedicled inferior turbinate flap, is a feasible technique that offers acceptable success rates due to the remarkable vascularity and thickness of the flap. The use of endoscopes allowed more precise a traumatic elevation of the flap posteriorly. The present technique differs from other previously described flap procedures in that it extends the posterior dissection to include a part of the mucosa of the inferior meatus in order to allow more free un-constrained rotation of the flap, and decrease the thickness of the pedicle so that we may not need to divide it in a second stage. This step would have been more difficult and less precise without the use of the endoscope. Previously operated turbinates are not suitable for this technique. Also the procedure may not be suitable if the perforation is very anterior or larger than 2 cm in diameter.
Keywords: Septum; Perforation; Endoscopic; Inferior turbinate flap
- Rhinology and Allergy
Session Introduction
Silvia Muriño
Parmenio Piñero Acute General Hospital, Argentina.
Title: Relationship between Immunodeficiencies, Allergy and Pathology of the Upper Airway

Biography:
ENT PhD and Allergy & Immunology practitioner, Parmenio Piñero Acute General Hospital (Buenos Aires City), F.A.S.O. Plenary member (Federación Argentina de Sociedades de Otorrinolaringología), A.O.C.B.A. Assistant Secretary, IAPO - Interamerican Association of Pediatric Otorhinolaryngology, American Academy of Otolaryngology-Head and Neck Surgery Intl Member, European Academy of Allergy & Clinical Immunology Intl Member
Abstract:
The respiratory system has defense mechanisms such as hair cells, Immune System, cough, sneezing, etc. Let's talk about the relationship between airway, allergy and immunodeficiency.
One of the most important substances to take into account is Histamine, both in its beneficial aspect and producing symptoms characteristic of these pathologies. IgE-mediated reactions, also present, involve mast cells and basophils.
The alteration of immunity and allergy is considered as a breakdown of the balance of the immune system. Let's not forget genetic and environmental factors (increased incidence in more urbanized communities)
We will also talk about the autonomic innervation that is so important to understand the symptomatology and its influence on the immune system and vice versa.
Arman Afrashi
Buca Seyfi Demirsoy State Hospital, Turkey.
Title: Pharyngolateral ferromagnetic prosthesis (PFP) for treatment of obstructive sleep apnea

Biography:
Abstract:
Obstructive sleep apnea is a disease consisting of episodes of partial or complete closure of the upper airway that occur during sleep and lead to breathing cessation defined as a period of apnea more than 10 s. Symptom include restlessness, snoring, recurrent awakening, morning head- ache and excessive day time sleepiness. Diagnosis of obstructive sleep apnea is based on sleep history and pol- ysomnography. Today the major treatment methods are continuous positive airway pressure, weight loss, positional therapy, oral appliances and different surgical procedures such as tracheostomy, nasal surgery, radiofre- quency of palatal region, soft palate implants, uvulophar- yngopalatoplasty, tongue base surgery, hyoid suspension, lateral pharyngoplasty, genioglossal advancement and maxillomandibular advancement.
In all of these surgical procedures except maxilloman- dibular advancement, the main problem is failure of pre- venting the collapse of lateral pharyngeal wall. In this new technique pharyngolateral ferromagnetic prosthesis will prevent the collapse of lateral pharyngeal wall during sleep.
Pharyngolateral ferromagnetic prosthesis: it contains two parts for each side of the pharyngeal part of the neck.
1. Internal part of prosthesis: it contains a fragmented thin part of a ferromagnetic material such as Iron (Fe), coated with biocompatible Silicone or another bio- compatible material.
2. External part of prosthesis: it contains a natural magnet with power between 6,000 and 10,000 Gauss. The external part of pharyngolateral ferromagnetic pros- thesis will use only during sleep in external part of the neck .
Surgical technique: patient will be in supine position and under general anesthesia during surgery. After inserting Davis-Boyle mouth gag, surgeon should make a 3-cm-long incision vertically in lateral wall of pharynx at the level of base of the tongue. Then surgeon should make dissection under mucosal and submucosal layers toward hypophar- ynx. After that he/she should insert the internal part of prosthesis and at the end close the incision . Then surgeon could perform the same procedure to the opposite side of the neck or perform unilaterally.
A few days after surgery patient should use the external part of the prosthesis in both sides of the neck during sleep. The magnetic power of external part of pros- thesis will pull the internal part of prosthesis and lateral hypopharyngeal wall together and this will prevent the collapse of lateral pharyngeal wall and obstructive attacks.
Lee Akst
Johns Hopkins University, USA.
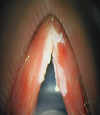
Title: Vocal Cord Leukoplakia: Management in the OR and Office

Biography:
Dr. Lee Akst is head of the Johns Hopkins Voice Center and is Director of the Division of Laryngology at the Johns Hopkins University Department of Otolaryngology-Head and Neck Surgery. The focus of his clinical practice is on management of voice disorders, with focus on office-based treatments and operative management of epithelial diseases such as vocal cord leukoplakia, papilloma, and early glottis cancer. He has lectured extensively on phonosurgical techniques, treatment of laryngeal leukoplakia, laryngopharyngeal reflux, and globus pharyngeus. He has been working with engineers at Johns Hopkins on novel robotic platforms to bringing robotic surgery into the endolarynx to aid microlaryngeal operative precision. Dr. Akst received his undergraduate and medical degrees from Yale University, did his Otolaryngology residency at the Cleveland Clinic, and completed his laryngology fellowship at Massachusetts General Hospital.
Abstract:
This presentation will comprehensively review evaluation and management of laryngeal leukoplakia. Though “white vocal fold lesions” are common, management remains challenging – doing ‘too little’ may allow precancerous lesions to progress, while doing ‘too much’ may create unnecessary dysphonia through scar. I will present a framework for management of leukoplakia which balances oncologic with functional outcomes, with the goal of achieving disease control without creating scar. State-of-the-art advances in care of leukoplakia will be emphasized, and surgical techniques discussed will include role of infusion, use of the KTP laser, and microflap resection of diseased epithelium. Advanced use of the KTP laser for office treatment of laryngeal dysplasia, an important part of my own practice and something which is only available in a limited number of centers worldwide, will be discussed as well, to include appropriate anesthesia techniques for office-based procedures. Epidemiology of leukoplakia, rates of progression to malignancy, and role of office-based biopsy will be reviewed.
Though focus will be on KTP laser strategies as these represent cutting edge approached to management of this disease, I will also discuss cold instrument and CO2 laser techniques so that the audience, regardless of the tools available to them in their own practices, will be able to transition techniques learned in this presentation to care of their own patients. Approaches to anterior commissure involvement, bilateral disease, and multiply recurrent dysplasia will be discussed through case presentations which should increase audience interest.
Learning Objectives: “At the completion of this presentation, participants should be able to:”
1. Understand the need to balance oncologic efficacy with functional outcomes in leukoplakia care.
2. Discuss treatment alternatives for laryngeal leukoplakia, emphasizing surgical techniques of KTP, CO2, and cold-instrument phonosurgery in the operating room and pulsed KTP laser treatment in an office setting.